A Research Spotlight From Breakthrough RESEARCH
The Beyond Bias Project
Building Evidence to Inform Practice for Provider Behavior Change Programming









Building Evidence to Inform Practice for Provider Behavior Change Programming









Breakthrough RESEARCH, with input from the United States Agency for International Development (USAID) and cross-sectoral implementing partners, developed research and learning agendas (RLAs) to strengthen two important areas of social and behavior change (SBC) programming: integrated SBC programming and provider behavior change (PBC).
The RLAs identify and document:
Provider behavior change (PBC) interventions go beyond clinical training to address provider attitudes, abilities, expectations, and resources available within their environment. They seek to positively influence provider behavior to improve the quality of services, enhance client experiences, increase demand for services, and increase uptake of commodities or adoption of healthier behaviors.

Beyond Bias was a project that sought to address provider bias by ensuring young people have access to empathetic, nonjudgmental, quality counseling and provision of a full range of contraceptive methods regardless of their marital status or parity.
Multiple barriers prevent a young person from accessing a safe method of contraception of their choice. Provider bias occurs at the last meter of care—the moment of consultation between youth and provider.
Beyond Bias used human-centered design (HCD), market segmentation, behavioral economics, and social and behavior change (SBC) principles to design and test innovative, scalable solutions that address provider biases.
A multidisciplinary approach that brought together experts in adolescent sexual and reproductive health (SRH), social and behavior change communication (SBCC), human-centered design, behavioral economics, and market segmentation to address this complex SRH problem.
By understanding what drives provider bias, small changes can be made to shift these biases and remove provider-related barriers.
The project was led by Pathfinder International, in collaboration with Camber Collective, YLabs, and RAND Corporation (and formerly the Behavioral Economics in Reproductive Health Initiative (BERI)), , with funding from the Bill & Melinda Gates Foundation.
November 2016 – June 2022
Burkina Faso, Pakistan, and Tanzania
With a mandate to disrupt the status quo, the project needed to assemble a multidisciplinary team to generate new solutions. Team members from different disciplines (e.g., social and behavior change communication, human-centered design) brought their own way of thinking.
The Beyond Bias team had to come together with intellectual empathy and humility to move beyond each discipline’s typical way of thinking and problem solving. This multidisciplinary process required frequent, intense engagement and collaboration across the project partners at key stages during the project lifecycle.
“Pathfinder put together a team that brings different perspectives to spark innovation. The innovation is the methodology and approach based on who was brought to the table.”
Provider bias was defined as a provider’s judgmental attitude or behavior toward adolescents in the provision of reproductive health services.
In different contexts, provider bias is driven by different things (e.g., sexual activity, age). Beyond Bias sought to look for key underlying drivers that are shared globally, allowing the project to develop solutions that can be adopted in multiple contexts.
What Are the Underlying Drivers That Shape Provider Behavior in Interpersonal Communication With Clients?
Synthesize what is currently known about healthcare provider bias; identify key factors likely to drive provider bias; identify gaps in the research/evidence base; and identify previously used quantitative measures of provider bias.
The literature review used the PRISMA—Preferred Reporting Items for Systematic Reviews and Meta-Analyses—checklist to outline specific steps and features of systematic reviews, and searched Google Scholar, PubMed, and PsychINFO databases.
A searchable matrix in Excel (Summary Tool) of available evidence.
Focus on perceptions about contraceptive use, role(s) of providers, bias influencers, and behavior change.
Twenty-nine expert informants were identified and contacted for semi-structured interviews. Experts included adolescent medical providers, global experts in sexual and reproductive health, academic researchers and thought leaders on adolescent development, and behavior change experts.
Interview summaries across five major categories:
Societal or community attitudes drive most documented provider bias. The most prevalent attitudes were expectations for:
The most consistent drivers of provider bias were:
A range of client characteristics influence interactions with providers:
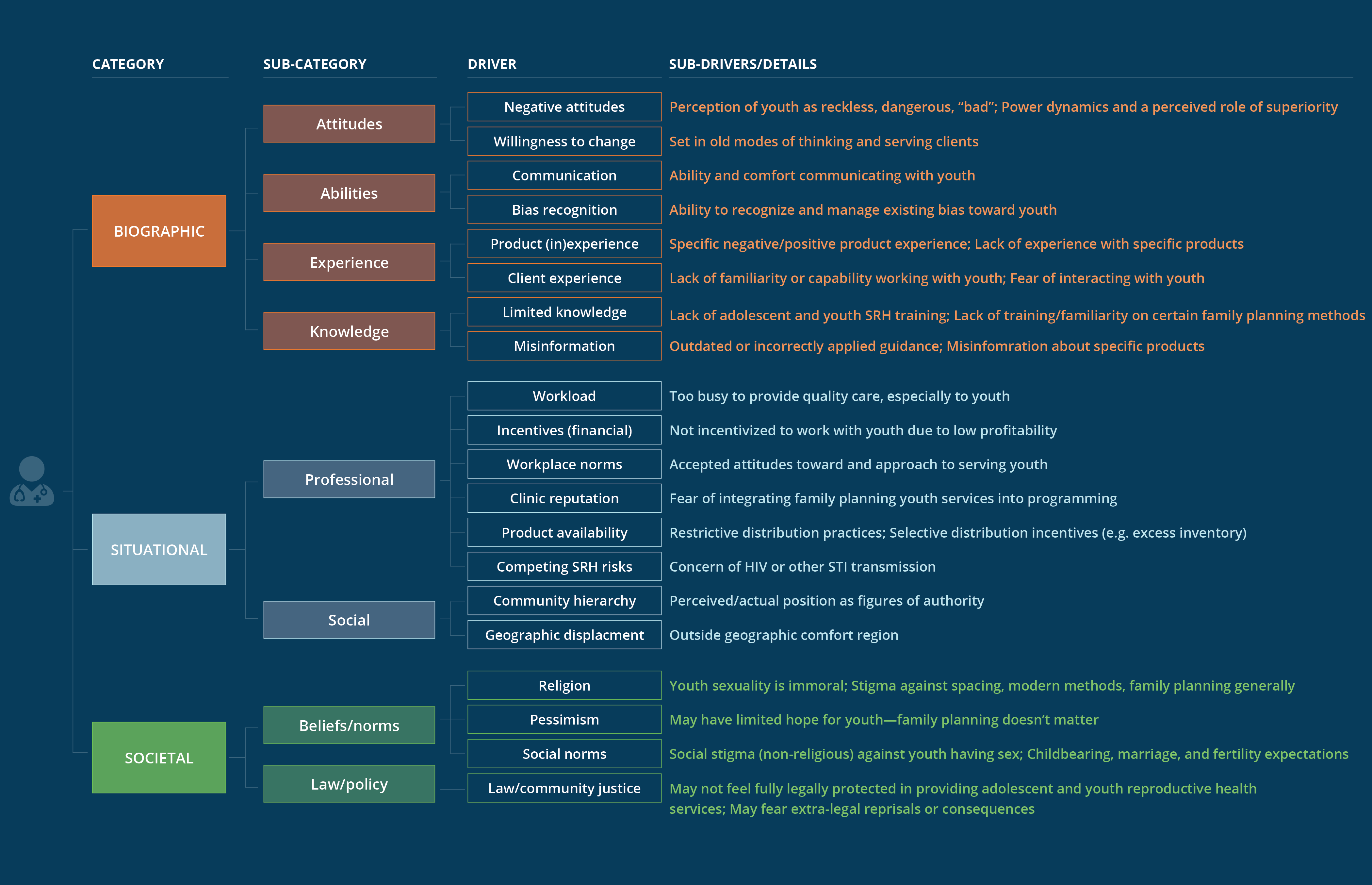
Beyond Bias developed a Provider Bias Driver Tree—an exhaustive set of drivers aggregated into three distinct categories:
These three distinct subsets of provider biases can be triggered, exacerbated, or ameliorated by specific adolescent demographic and behavioral traits.
How do the underlying drivers shape provider profiles?
Investigate the relative influence of different types of bias for each provider so that the data can be analyzed to identify the most prevalent influencers and types of bias for different segments of the provider population.
Camber Collective, in collaboration with in-country market research firms.
811 providers:
A quantitative survey captured demographic factors, focusing more on attitudinal and behavioral characteristics to develop empirically derived segments of provider profiles within each country.
Several types of questions and data collection methods were designed to measure provider bias. These include:

Well-trained, though emotionally disconnected from youth
Aware of adolescent and youth sexual and reproductive health practices, but somewhat biased and relatively unsympathetic for youth
Generally open-minded and youth friendly, but distrustful of modern methods and independent women
Most connected with young clients, though also prone to believe they know what’s best
Well-intentioned, and though somewhat misinformed, exhibit overall high-quality youth service

Busy older doctors who, despite some progressive attitudes, show strong marital and parity bias
For program managers, trainers, and implementers to understand their target providers and tailor their engagement.
A country-specific classification tool to accurately assess which segment a provider is best aligned and a segmentation adaptation pathway.
Manifestation of Bias in Tanzania
“I have too many patients and too little space. Sometimes women deliver on the floor because we don’t have enough tables.”
Which Intervention(s) or Combinations of Interventions Are Most Important to Improving the Quality of Provider Counseling?
How Did the Project Identify Provider Profiles?
Develop a series of solutions to help minimize provider bias.
YLabs led qualitative design research in collaboration with Pathfinder International.
Providers, young people, and other health system stakeholders.
Design research methodologies including interviews, observations, roleplay, and participatory research activities to investigate provider biases and behavior toward young women.
More than 100 ideas were generated by all partners.
Conduct rough prototyping sessions to fail early and learn directly from users to foster rapid iteration of identified solution concepts.
The key goals of rough prototyping are to:
Ylabs, in collaboration with Pathfinder International.
97 healthcare providers and 22 youth (and a few mothers-in-law) in Burkina Faso, Pakistan, and Tanzania.
Through rough prototyping—a method in the human-centered design process—a small number of essential questions about desirability and feasibility were tested for each solution concept.
Conducted live prototyping to rapidly design, test, and refine potential interventions.
YLabs and Pathfinder International.
Potential solutions were assessed and advanced based on the following core criteria, centered around solutions that could be taken to scale:
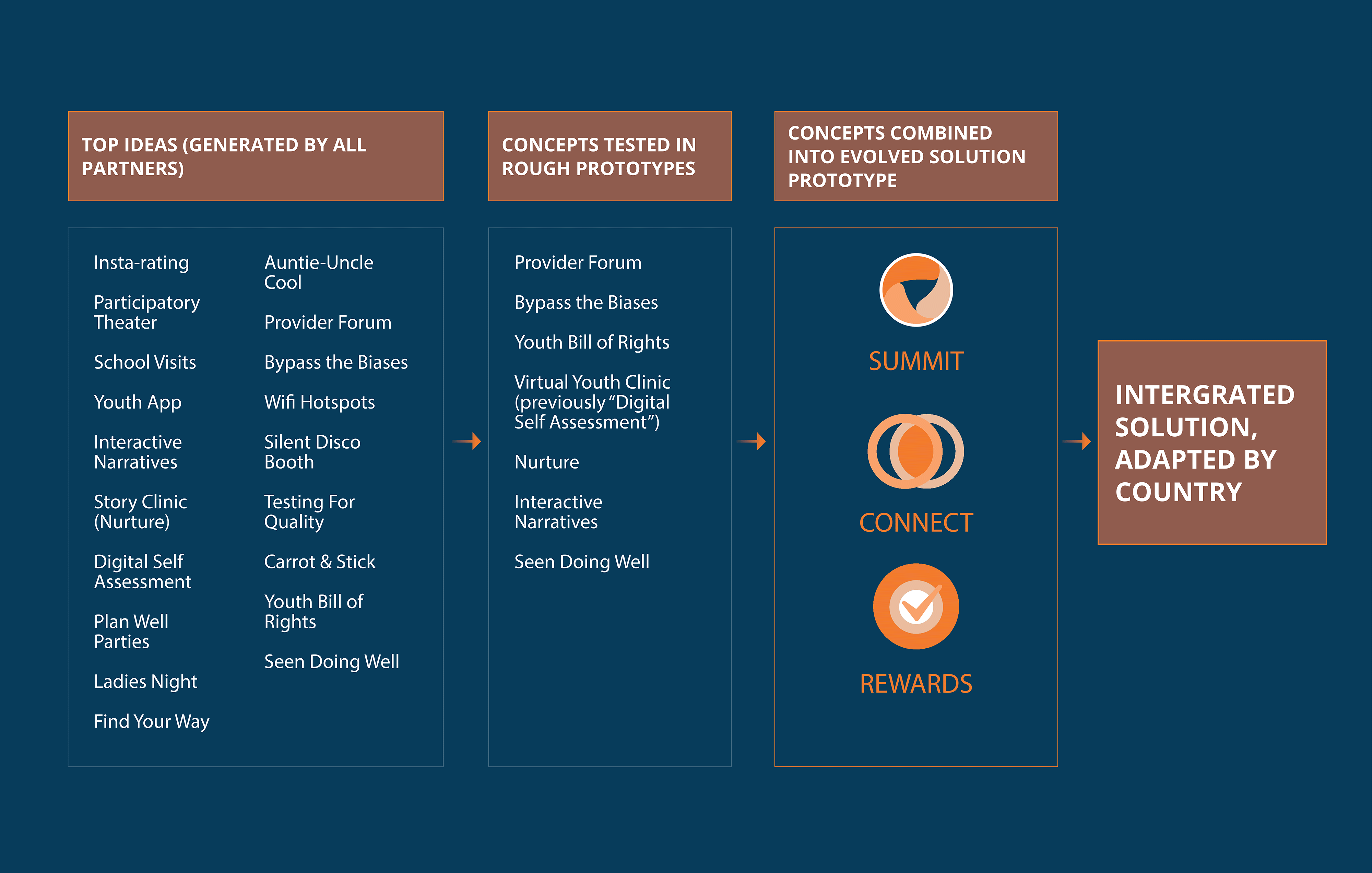
Beyond Bias designed a three-part behavior change strategy intervention for providers with six intended outcomes that address provider bias toward adolescent sexual and reproductive health.
Summit
Connect

Rewards
A three-part, adaptive solution to address provider bias.
Story-driven event with providers to:
“It’s true that there may be gaps in training, but the problem really lies within. Today I came to understand that sometimes my services to youth can be changed by my own bias.”
Built a professional community—connecting providers to one another—through a multiweek program of texts, videos, and information over WhatsApp, with a new theme each week.
“We felt like a family. It is a safe space where we can freely express whatever we think. Even our life stories were shared on the forum. I didn’t fear that someone will criticize or reprimand me. Through Connect I learned many new things. I felt valued on Connect.”
Used social reinforcement for progress as an incentive for providers. Facilities received report cards with performance data and recommendations for improvement. High-improvement facilities received public recognition for their progress.
“I changed my perspective and attitude towards young clients. My priority is serving youth just after the moment I knew my efforts would be recognized.”
Sept. 2019-Feb. 2020; Sept. 2020-Aug. 2021
Implement the Beyond Bias model across all three countries (Burkina Faso, Pakistan, and Tanzania), documenting experiences to contribute to the evidence on how to successfully implement a provider-focused intervention for adolescent sexual and reproductive health services.
Pathfinder International
Note: Half of clinics were randomized to receive the Beyond Bias intervention. After implementing the intervention for one month in Burkina Faso, six months in Pakistan, and four months in Tanzania, the COVID-19 pandemic required a pause in all implementation activities. The pause lasted for six months across all three countries. Some provider turnover occurred during this period and limited clinic attrition.
Summit is a one-day, story-driven, in-person event that activates providers’ self-awareness of their own biases and empathy for young people’s needs. It is designed to facilitate dialogue and support providers in creating action plans for shifting their biases. Each event engages up to 40 providers and includes testimonials and interactive group exercises. The content is proportionally tailored to the provider segments in that country.
Note: Due to the pause in implementation early in the COVID-19 pandemic, the project included a “refresher Summit” event in all countries after the pause.
Connect is an ongoing, interactive peer-support forum for knowledge sharing and learning. Providers begin Connect the week after they attend Summit and are grouped with the same cohort they met during Summit. Connect activities can be conducted in person, virtually using WhatsApp or a similar service, or as a blended model. Connect consists of two phases—an intensive phase and a continuous learning phase—though the approach is meant to be flexible and thus timing and modalities can be adapted based on the team’s needs. The intensive phase as described here is eight to ten weeks long and is completed before the first quarterly Rewards event (see next column). The continuous learning phase begins in month 4, after the first round of Rewards events, and ends in month 12. During the continuous learning phase, providers are engaged once or twice a month, depending on the intervention delivery method.
Rewards is a growth-oriented, non-monetary, performance-based incentive for clinics assessed through client feedback on provider behavior. Facilities receive quarterly report cards from the Beyond Bias team with performance data and recommendations for improvement; those with high improvement scores receive public recognition for their progress during quarterly events with their fellow providers and the Beyond Bias team. Through prototyping, the Beyond Bias team learned what types of non-financial recognition were most exciting to providers and were able to test different formats for delivering that recognition. The project also learned that rewarding facilities based on an absolute grading scale seemed to be less motivating than recognizing facilities that had achieved improvements over time (for example, don’t just recognize the “most-valuable player” but also the “most-improved player”).

During Summits in Pakistan, providers were introduced to the Six Principles of Unbiased Care, derived from the World Health Organization’s quality of care principles and received posters, a Six Principles booklet, and other materials. Through a guided exercise and use of “commitment cards”, each provider identified at least one principle to work on moving forward. Summits ended with each provider receiving a commitment pin bearing the message “I support the choices of young people” from guest experts in the room.
Providers in Tanzania expressed a preference for a blended version of Connect because they wanted a mix of digital and in-person activities. For the digital activities, providers were divided into two digital Connect WhatsApp groups (one group had 75 members; the other group had 66 members). An additional WhatsApp group was formed for facility managers who ran in-person Connect sessions. For eight weeks, the WhatsApp groups received tailored messages around one topic per week from the Beyond Bias team to help improve clinical care and reduce bias for young people.
The topics were:
The digital Connect sessions were complemented by simultaneous in-person activities. During the project’s first quarter, designated, trained facility managers led providers through one in-person meeting per week for six weeks. Topics included a refresher training on provider bias, youth client and provider experience case studies, true/false technical reviews, and peer exchanges.

The Burkina Faso team identified Reward-winning facilities based on facility report card scores. Awards were given to the highest-scoring facilities based on overall marks in the quarter, and to facilities and providers with the most-improved scores between quarters. Rewards events included time for celebration as well as reflection and sharing of best practices with other facility managers and regional health representatives. Participants enjoyed a sense of healthy competition that developed between facilities, with all pledging to “be on top” in coming quarters. Providers said they particularly appreciated receiving personal report cards and being publicly recognized in the presence of their superiors.
Does improving the behaviors/practices of health providers influence the quality of care provided?
What are the most effective SBC approaches to enable, motivate, or facilitate providers to provide respectful, client-centered care?
Sept 2020 – Aug 2021
Evaluate the impact of the intervention program in all three countries on provider behavior and attitudes and patient-centered care for family planning services.
RAND Corporation
Note: Some monitoring data (for instance, facility service data and exit survey data) were collected throughout project implementation, while other data were collected specifically for end-of-project evaluation purposes during the final two months of implementation (for example, mystery client data, provider survey data, and qualitative interview data).
Main outcome domains included: (1) provider attitudes/beliefs; (2) patient-centered family planning care; (3) family planning method received; and (4) perceived treatment (see figure), and were measured using a mix of quantitative and qualitative methods.

Note: As the Beyond Bias intervention was targeted at health providers with the intention to make them less biased, we expected to see direct changes in provider attitudes and beliefs. These changes, in turn, should result in changes in patient-centered family planning (FP) care, which should then affect the family planning methods that clients receive. Finally, the combination of patient-centered family planning care and methods received should affect how clients perceive treatment of family planning services obtained from their interactions with their provider.
Summary of results: Compared with the control group, the providers who took part in the Beyond Bias intervention reported more empathetic, nonbiased attitudes toward the target groups and counseled young clients on the full range of methods more frequently. Young clients counseled by these providers reported improved perceptions of how they were treated during family planning visits (see figure above). However, the intervention was not associated with the extent to which the quality of counseling or the types of contraceptive methods offered depended on client demographic characteristics such as age, marital status, and parity. Nor did it lead to an increase in uptake of an expanded range of contraceptive methods for adolescents and youth who came into the clinic.

The intervention reduced biased provider attitudes and beliefs with respect to age, marital status, and parity in all three countries. Effects were most prominent for beliefs about how to provide family planning care to clients and underlying beliefs about clients’ lives and intentions. For example, in an analysis of data from all three countries together, providers were significantly less likely to report imposing method restrictions because a client was “too young” (23 percentage-point difference), unmarried (7 percentage-point difference), or did not have children (15 percentage-point difference).

Beyond Bias significantly improved all patient-centered family planning care outcomes. The largest and most prominent improvements came from the way clients were counseled and the way they felt they were treated in Tanzania and Pakistan. In pooled analysis using the mystery client data, clients at intervention clinics were not only counseled on more methods than at control clinics but were also more likely to be asked essential questions and given more information about the methods. Burkina Faso saw relatively little effect.
Beyond Bias found limited evidence of change for a client receiving a method and method of choice or method mix in the study sites. This lack of change is partly explained by very high rates of these outcomes in the control group (more than 91% of clients in the control group in Tanzania and Burkina Faso, and 82% in Pakistan received a modern method), leaving very little room for improvement.

Beyond Bias improved clients’ perceived treatment by providers (for instance, clients were not judged or scolded by a provider or made uncomfortable during a clinic visit and were likely to recommend the clinic to a friend) compared to control sites. Positive, significant pooled effects were driven by improvement in Tanzania and Pakistan, with little change in Burkina Faso on these outcomes (partly due to health system-level challenges). For example, in Tanzania clients experienced a 50% reduction in the likelihood of being judged or scolded by a provider.
Qualitative results support quantitative evidence of attitudinal changes among providers following participation in Beyond Bias. Providers spoke about how they no longer refuse or limit services for certain types of clients—most commonly, young women, unmarried women, and nulliparous women:
“We had the myths that we shouldn't give family planning services to newly married couples and young-age people… But now we give family planning services to 17 years and under age people. Those who are young need family planning services too.”
Human resource constraints made it challenging to fully participate in the intervention:
“During the Connect sessions, if you are the only one providing the service, you want to follow the Connect but … you cannot follow because you are busy doing something else in the delivery room.”
“In Tanzania, the Beyond Bias initiative achieved great buy-in from the government, specifically from the Ministry of Health, as a novel approach to address provider bias… The Ministry of Health played a key role in giving what we call social permission to health care providers to serve adolescents and youth without the fear of community backlash… In this case, also in Tanzania, the use of positive deviants gave us a good step towards the success of the implementation because the positive deviants—who are converted health care providers… who are giving the services to adolescents without bias, without being judgmental—took a great lead in helping the others also change and perform better. All these factors give health care providers the will to do better.”
“As a result of some of our monitoring data, we did see a few important learnings and made some adaptations to better strengthen the overall Beyond Bias approach. For example, our monitoring data suggests that higher Connect participation often resulted in higher Reward scores, which were associated with [better] quality of care… We used this information to motivate provider participation in Connect by engaging facility managers [and sharing] some of the data that we have seen. We were able to increase Connect participation by over 10 percentage points from the first quarter all the way to the final quarter.”
“My greatest surprise was the challenges of measuring bias, the intricacies of it, and how you disentangle system issues from our own issues… The six months [COVID] pause period was a blessing for us… we spent those six months trying to go back to the drawing board and try to revamp a tool for us to be able to detect bias… we made some improvements, we had some learnings, but I cannot really emphasize enough how much the [measurement] area needs help. We need more work in this area.
“Another element that is not much of a surprise, but rather a point of reflection, is the level of empathy I now feel towards providers. Of course, this project was about addressing biases and how it acts as a barrier for youth access to contraception, which is still valid, and I am sold to that mission. But really, after years of talking and engaging with providers I feel like I have more consideration and respect for them. And I generally think as a field we need to think more about and be more careful about how we communicate with them and how we assess their work.”
For more information about Beyond Bias, please contact beyondbias@pathfinder.org or visit the Beyond Bias project webpage.
For more information about Breakthrough RESEARCH visit the Breakthrough RESEARCH project.
This Beyond Bias case study was developed by Sanyukta Mathur and Krista Granger, Population Council, with input from Kamden Hoffmann, Population Council, Rachel Yavinsky and Heidi Worley, Population Reference Bureau (PRB). It was designed by ProGraphics in consultation with Nancy Andrews, Creative Director at PRB, and edited by Nancy Matuszak, PRB.
The case study was developed with the assistance of Pathfinder International and the Beyond Bias project. Thank you to Lydia Murithi, Beyond Bias Project Director. Thanks also to Marta Pirzadesh, Senior Technical Advisor, AYSRHR; with Mohamad (Bram) Brooks, MEL Lead/Senior Manager; and Cecelia Angelone, Senior Program Officer for their guidance and critical input.
This website is made possible by the support of the American people through the United States Agency for International Development (USAID). The Breakthrough awards are supported by USAID’s Office of Population and Reproductive Health, Bureau for Global Health, under Cooperative Agreements: #AID-OAA-A-17-00017 and #AID-OAA-A-17-00018. Breakthrough ACTION is based at the Johns Hopkins Bloomberg School of Public Health’s Center for Communication Programs. Breakthrough RESEARCH is based at Population Council. The contents of this website are the sole responsibility of Breakthrough ACTION and Breakthrough RESEARCH. The information provided on this website is not official U.S. Government information and does not necessarily represent the views or positions of USAID, the United States Government, Johns Hopkins University, or Population Council. All rights reserved.
This page is hosted by Population Reference Bureau. Privacy Policy